About Half of Infertility Cases Are Due to Male Factors
Infertility is often assumed to be caused by issues on the female side, but in reality, approximately half of infertility cases are due to male factors. At our clinic, board-certified urologists perform precise examinations and provide scientifically based treatments to diagnose and treat male infertility.
Who We Treat
We offer care for men experiencing the following issues:
- Abnormal semen analysis results (low sperm count, low motility, etc.)
- Erectile dysfunction or ejaculation disorders
- Azoospermia or oligozoospermia
- Decreased reproductive function due to aging or lifestyle factors
Our Approach
- Comprehensive evaluation of male reproductive function, including semen and hormone tests
- Recommendations for medication, lifestyle modifications, or SGF® (stem cell-derived treatment) as needed (private-pay option)
- Consultations and follow-up by experienced urologists and regenerative medicine specialists
What Is Male Infertility?
Infertility is defined as the inability to achieve pregnancy after more than two years of regular, unprotected intercourse. When the cause lies with the male partner, it is termed male infertility.
Diagnosis of Male Infertility
The diagnostic process includes:
- Medical interview and physical examination (e.g., testicular size assessment)
- Hormone tests, scrotal ultrasound, and genetic testing
- The most critical test is the semen analysis.
This test evaluates sperm count, concentration, motility, and semen volume. Values below standard thresholds may indicate reduced fertility.
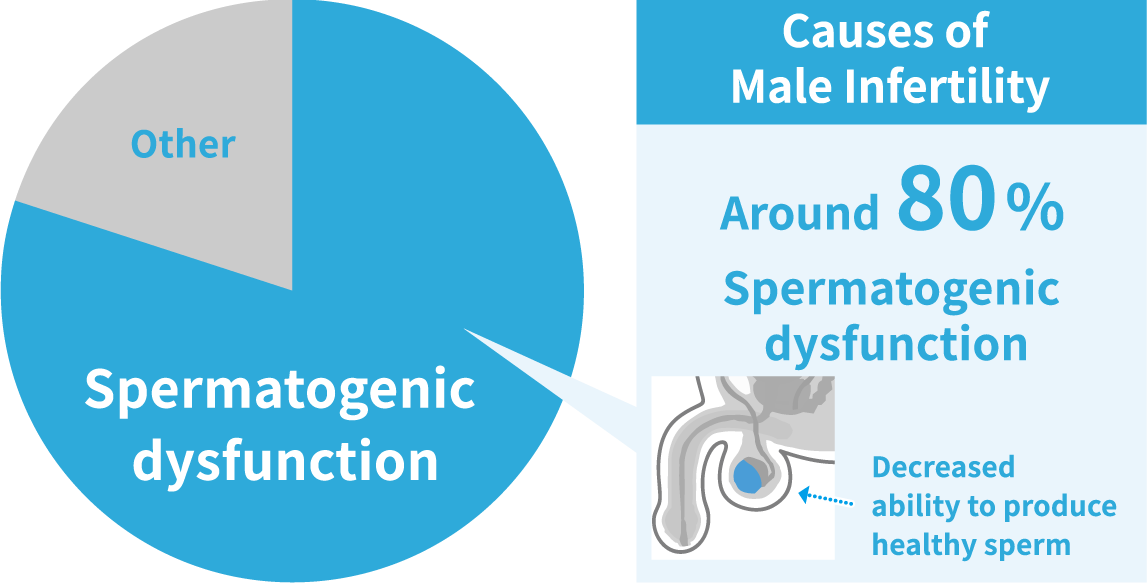
Causes of Male Infertility
About 40–50% of infertility cases involve male factors. Around 80% of male infertility is due to spermatogenic dysfunction, and about half of these are idiopathic (unknown cause).Primary Classifications:
- Spermatogenic dysfunction: Low count, poor motility, or abnormal
- Sexual dysfunction: Erectile or ejaculation issues
- Obstructive causes: Sperm is produced but cannot exit the body
Causes of Spermatogenic Dysfunction
A condition in which the testicles cannot produce sperm effectively.
- Congenital factors: Chromosomal abnormalities (e.g., Klinefelter syndrome), Y-chromosome microdeletions
- Varicocele: Enlarged veins increase testicular temperature and impair sperm production
- Undescended testes or orchitis
- Cancer or anticancer treatments (e.g., chemotherapy, radiation)
- Pituitary gland disorders affecting hormone production
Male Infertility Testing
Semen Analysis
This test is available by appointment only. Semen samples can be collected at the clinic or at home in a more comfortable environment. (If collected at home, please bring it to the clinic within 30 to 60 minutes.) We provide sterile specimen containers in advance or ship them (at your own expense). The analysis takes approximately 15 to 20 minutes.
Semen analysis evaluates volume, sperm concentration, motility, and morphology, and compares these values with the lower reference limits established by the WHO (World Health Organization).
The sperm concentration refers to the number of sperm per milliliter of semen. Among these, the concentration of sperm showing forward motility is referred to as the progressive motile sperm concentration. This value is most closely related to the Sperm Motility Index (SMI).
An SMI score of 80 or above is considered favorable. A higher SMI generally correlates with a higher pregnancy rate.
| SMI | Progressive Motile Sperm Concentration (×10⁶/ml) | Sperm Concentration (×10⁶/ml) | Progressive Motility Rate | |
| WHO Lower Reference Limit | 80 | 4.8 | 15 | 32% |
Our Clinical Cases
Testicular Injections to Improve Sperm Quality
SGF® (deciduous tooth pulp-derived stem cell conditioned medium) is directly injected into the testicles to improve sperm count and motility.
Unlike testosterone therapy, this is a biologically derived treatment aimed at restoring natural testicular function.
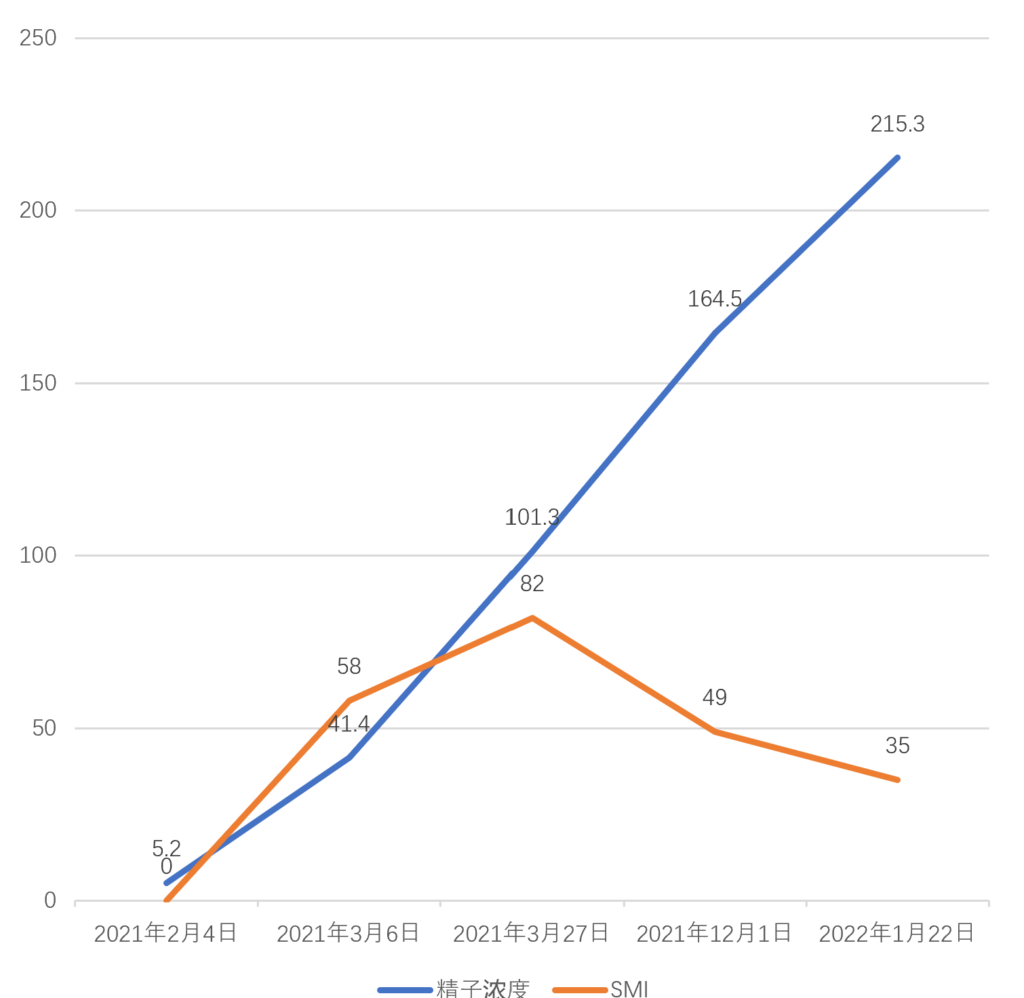
Case 1: 58-year-old male
Feb 4, 2021: Sperm concentration 52,000/ml, SMI 0
Dec 2020 – Mar 2021: 10 testicular injections
Mar 27, 2021: Sperm concentration 1,013,000/ml, SMI 82
Jan 22, 2022: Sperm concentration 2,153,000/ml, SMI 35
About Semen Analysis
The Importance of Semen Analysis
In recent years, declining sperm quality in adult men has been frequently cited as one of the contributing factors to Japan’s declining birthrate and aging population.Although semen analysis is commonly associated with infertility treatment, it is also a highly valuable tool for men to understand their overall physical and even mental health.Knowing the condition of your sperm can provide insight into whether your daily lifestyle habits are healthy and balanced.
What often needs to be improved is your lifestyle—especially diet.Maintaining a good balance of diet, sleep, and exercise is key. However, long-standing poor habits can impair the function of the testicles, which are responsible for sperm production.Currently, conventional medicine does not offer a definitive treatment for impaired testicular function.In most cases, improvements are attempted through nutritional counseling, often including zinc supplementation.
At our clinic, we aim to restore testicular function itself using SGF® (deciduous tooth pulp stem cell conditioned medium).
When Semen Analysis Results Are Unsatisfactory
As mentioned, semen parameters fluctuate. It’s not uncommon for a poor first result to be followed by a normal one on re-testing.Clinical guidelines recommend performing at least two semen analyses within a 3-month period. We also advise retesting when initial results are suboptimal.Semen quality is strongly influenced by lifestyle.Smoking and obesity are well-known risk factors that can negatively affect semen quality.
How to Improve Sperm Quality
Vitamins B12, E, C, zinc, and folic acid have been shown to improve semen quality. Aim for a well-balanced diet.Here are some key points to consider:
- Avoid Pressure on the Testicles
-
Avoid prolonged sitting, which puts pressure on the testicles. Take breaks every hour to improve circulation.
- Avoid Overheating the Testicles
-
Sperm are sensitive to heat. Avoid long baths or extended sauna use. Wear breathable underwear like boxers, and avoid placing laptops on your lap.
- Avoid Smoking
-
Smoking is known to deteriorate sperm quality. Quit smoking if possible.
- Maintain a Healthy Weight
-
Obesity is another known risk factor for poor sperm health. Maintain a healthy weight.
- Avoid Excessive Abstinence
-
Avoid prolonged abstinence. Retained older sperm can oxidize and impair motility. An ideal abstinence period is 3–4 days.
- Exercise Regularly
-
Exercise regularly to improve pelvic circulation. Walking, light jogging, yoga, and stretching are all beneficial.
Patent Technology
Our clinic holds a patent (No. 6830286) for a testicular function enhancement agent using SGF® (deciduous tooth pulp stem cell conditioned medium).
Male Infertility Treatment with SGF®
Our clinic offers localized testicular injection therapy using SGF® (Deciduous Tooth Pulp Stem Cell Conditioned Medium) as a self-funded treatment.The injection is administered directly into the testicles using an ultra-fine needle, resulting in minimal discomfort.The procedure is quick and places very little strain on the body.
Expected Benefits of SGF® Injection
- Promotes the repair of testicular cells
- Activates and increases sperm production
- Enhances testosterone secretion
- Improves Sperm Motility Index (SMI)
- May help prevent lifestyle-related diseases
For Those Considering Male Infertility Treatment
If you are struggling with infertility or have undergone tests at other clinics without seeing improvement, we encourage you to consult us.
Our physician, specializing in regenerative medicine and urologic oncology, will provide evidence-based diagnosis and treatment, offering the most suitable therapeutic approach to support your path to conception.

